Utilization of a pre-designed structure offers several advantages. Clear presentation of financial information promotes patient satisfaction and reduces billing inquiries. Consistent documentation improves efficiency in claims processing and minimizes errors, ultimately leading to faster reimbursements. Furthermore, standardized forms simplify compliance with industry regulations and ensure accurate record-keeping for auditing purposes. These benefits contribute to a smoother financial process for both patients and providers.
This foundational understanding paves the way for a deeper exploration of related topics, including the creation, customization, and effective use of these essential documents within the healthcare revenue cycle. Further discussion will encompass best practices for design and implementation, legal considerations, and the evolving role of technology in optimizing billing processes.
1. Standardized Format
Standardized formatting is crucial for medical billing statement templates. Consistency ensures clarity for patients, streamlines processing, and simplifies compliance. A structured approach promotes efficiency and reduces errors throughout the revenue cycle.
- Consistent LayoutA predictable layout ensures patients can easily locate key information such as dates of service, procedure codes, and payment details. For example, consistently placing patient demographics in the upper right corner and payment instructions at the bottom facilitates quick access to vital information. This consistency reduces confusion and improves patient experience.
- Uniform TerminologyUsing standardized medical codes (e.g., CPT, HCPCS) and descriptions ensures consistent communication between providers, payers, and patients. For instance, using the correct code for an office visit eliminates ambiguity and ensures accurate billing. This uniformity minimizes claim rejections and accelerates reimbursements.
- Defined Data FieldsClearly defined fields for specific data points, such as patient name, insurance information, and charges, ensure accurate data capture and processing. This structured approach minimizes errors and facilitates electronic data exchange. Consistent data fields also simplify analysis and reporting.
- Accessibility ConsiderationsStandardized formats can incorporate accessibility features, such as large font sizes and clear language, to accommodate patients with diverse needs. This inclusivity ensures all patients can understand their billing statements. Accessible design demonstrates a commitment to patient-centered care.
By adhering to a standardized format, medical billing statement templates promote transparency, efficiency, and accuracy in healthcare financial processes. This structured approach benefits both patients and providers, contributing to a smoother revenue cycle management.
2. Clear Itemization
Clear itemization forms the cornerstone of a transparent and effective medical billing statement template. It provides patients with a detailed breakdown of services rendered, ensuring they understand the rationale behind each charge. This transparency fosters trust and reduces the likelihood of billing disputes. A clearly itemized statement distinguishes individual procedures, consultations, tests, and medications, preventing confusion stemming from bundled or unclear charges. For example, a statement might list a specific office visit, an electrocardiogram (ECG), and a blood test as separate line items with corresponding charges, rather than grouping them under a generic “consultation fee.” This granular approach empowers patients to verify the services received and their associated costs.
The practical significance of clear itemization extends beyond patient understanding. It simplifies the claims processing and review process for insurers. Itemized bills facilitate accurate coding and billing, reducing claim rejections and accelerating reimbursements. Furthermore, clear itemization aids in internal auditing and financial analysis. By tracking individual services and their associated costs, healthcare providers can identify areas for cost optimization and improve revenue cycle management. Consider a scenario where numerous claims are rejected due to unclear billing for a specific procedure. A clearly itemized statement allows for rapid identification of the coding error, enabling prompt correction and resubmission, thus preventing revenue loss.
In summary, clear itemization is not merely a best practice; it is an essential component of a well-designed medical billing statement template. It promotes transparency, strengthens patient-provider relationships, streamlines insurance processing, and facilitates efficient financial management. Challenges may arise in accurately coding and describing complex procedures, but the benefits of clear itemization far outweigh the effort required to implement it effectively. This meticulous approach ultimately contributes to a more robust and ethical healthcare financial system.
3. Accurate Data
Data accuracy within medical billing statement templates is paramount for efficient revenue cycle management and positive patient-provider relationships. Inaccurate data leads to claim rejections, delayed reimbursements, and patient dissatisfaction. A commitment to accuracy ensures compliance, minimizes financial losses, and fosters trust.
- Patient DemographicsCorrect patient information, including name, address, date of birth, and insurance details, is fundamental. Errors in these fields can cause claim denials and delays. For instance, a misspelled name or incorrect insurance ID number can lead to a rejected claim. Accurate demographic data ensures proper identification and facilitates smooth claims processing.
- Service Codes and DescriptionsAccurate Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes are crucial for appropriate reimbursement. Inaccurate codes can result in underpayment or denial of claims. For example, using a code for a basic office visit when a more complex consultation occurred leads to lost revenue. Precise coding reflects the services provided and ensures accurate billing.
- Dates of ServiceAccurate dates of service are essential for tracking patient care and determining appropriate billing. Incorrect dates can lead to claim discrepancies and delays. For example, if the date of service doesn’t match the patient’s medical record, the claim may be flagged for review. Correct dates ensure proper alignment with medical records and facilitate timely processing.
- Charge AmountsAccurate charge amounts reflect the agreed-upon fees for services rendered. Errors in charge amounts can lead to overbilling or underbilling, both of which have negative consequences. Overbilling can damage patient trust and lead to legal issues, while underbilling results in lost revenue. Accurate charges ensure appropriate reimbursement and maintain financial integrity.
These interconnected data points form the foundation of a reliable medical billing statement template. Data accuracy is not merely a technical detail but a core ethical and operational requirement. It directly impacts revenue cycle efficiency, patient satisfaction, and compliance with healthcare regulations. Maintaining accurate data through rigorous verification processes and system integrations is crucial for financial stability and positive patient-provider relationships.
4. Patient Information
Accurate and comprehensive patient information is crucial for the efficacy of a medical billing statement template. It ensures proper identification, facilitates communication, and supports accurate claims processing. Without correct patient information, statements become ineffective, leading to delays, errors, and potential financial losses. This section explores the key facets of patient information within the context of medical billing.
- Demographic DataDemographic data forms the foundation of patient identification. This includes the patient’s full legal name, date of birth, address, and contact information. Accurate demographic data ensures that the statement reaches the correct recipient and enables providers to contact the patient regarding billing inquiries. For instance, an incorrect address can lead to a returned statement and delayed payment. Furthermore, accurate demographic information is essential for insurance verification and claims processing.
- Insurance InformationInsurance details are essential for accurate billing and reimbursement. This includes the patient’s insurance provider, policy number, group number, and the name of the insured. Accurate insurance information ensures that claims are submitted to the correct payer, minimizing denials and delays. For example, an incorrect policy number can lead to a rejected claim, requiring resubmission and delaying payment. This information is crucial for determining patient responsibility and coordinating benefits.
- Medical Record Number (MRN)The MRN is a unique identifier assigned to each patient within a healthcare system. Including the MRN on the billing statement links the statement to the patient’s medical record, facilitating accurate tracking and reconciliation of services rendered. This connection is vital for internal audits, data analysis, and ensuring that the billing information aligns with the documented medical care. Accurate MRN usage streamlines internal processes and minimizes discrepancies.
- Responsible Party InformationIn cases where the patient is a minor or unable to manage their financial affairs, the responsible party’s information is necessary. This includes their name, relationship to the patient, address, and contact information. Including this information ensures that the bill reaches the individual responsible for payment, avoiding delays and confusion. Accurate responsible party information is particularly important for pediatric and geriatric care.
These interconnected elements of patient information are essential for a functional medical billing statement template. Accurate and complete patient data ensures efficient processing, minimizes errors, and contributes to a positive patient experience. By prioritizing data integrity, healthcare providers can optimize revenue cycle management and maintain strong patient relationships. Ultimately, attention to these details strengthens the financial health of the healthcare system.
5. Payment Details
Inclusion of comprehensive payment details within a medical billing statement template is crucial for facilitating timely and accurate payment processing. Clear payment instructions empower patients to understand their financial responsibility and simplify remittance, contributing to a more efficient revenue cycle. This section explores key facets of payment details and their impact on the overall effectiveness of a medical billing statement.
- Total Amount DueClearly stating the total amount owed is fundamental. This prominent figure represents the patient’s financial obligation after insurance adjustments and other deductions. A clear presentation of the total due eliminates ambiguity and ensures the patient understands the precise amount to be paid. For example, a statement should clearly differentiate between the total charge, insurance payments, adjustments, and the final patient responsibility.
- Payment Methods AcceptedListing accepted payment methods provides patients with flexibility and convenience. This typically includes options such as online payments, mail-in checks, and in-person payments. Providing multiple options accommodates diverse patient preferences and encourages timely payment. For instance, offering online payment portals simplifies the process and reduces processing time compared to traditional mail-in methods. Statements might also include details for paying via phone or through third-party payment platforms.
- Payment Due DateA clearly specified due date sets expectations and encourages prompt payment. This date establishes the timeframe within which payment should be received to avoid late fees or other penalties. Clearly presenting the due date helps patients prioritize payment and avoid potential negative consequences. Statements may also include information regarding grace periods or payment plan options, if available.
- Payment InstructionsDetailed payment instructions guide patients through the payment process. This includes specific instructions for online payments, mailing addresses for checks, and details for in-person payments. Clear instructions minimize confusion and ensure accurate processing. For example, instructions for online payments might include a website URL and specific steps to access the payment portal. Instructions for mailing payments should include the correct mailing address and any required accompanying documentation, such as a remittance slip.
These interconnected payment details contribute significantly to the effectiveness of a medical billing statement template. Clear and comprehensive payment information empowers patients to fulfill their financial obligations efficiently, contributing to a smoother revenue cycle for healthcare providers. Well-designed payment details ultimately benefit both patients and providers, fostering transparency and facilitating timely payments. By prioritizing clear communication of payment information, healthcare organizations can optimize revenue cycle management and enhance patient satisfaction.
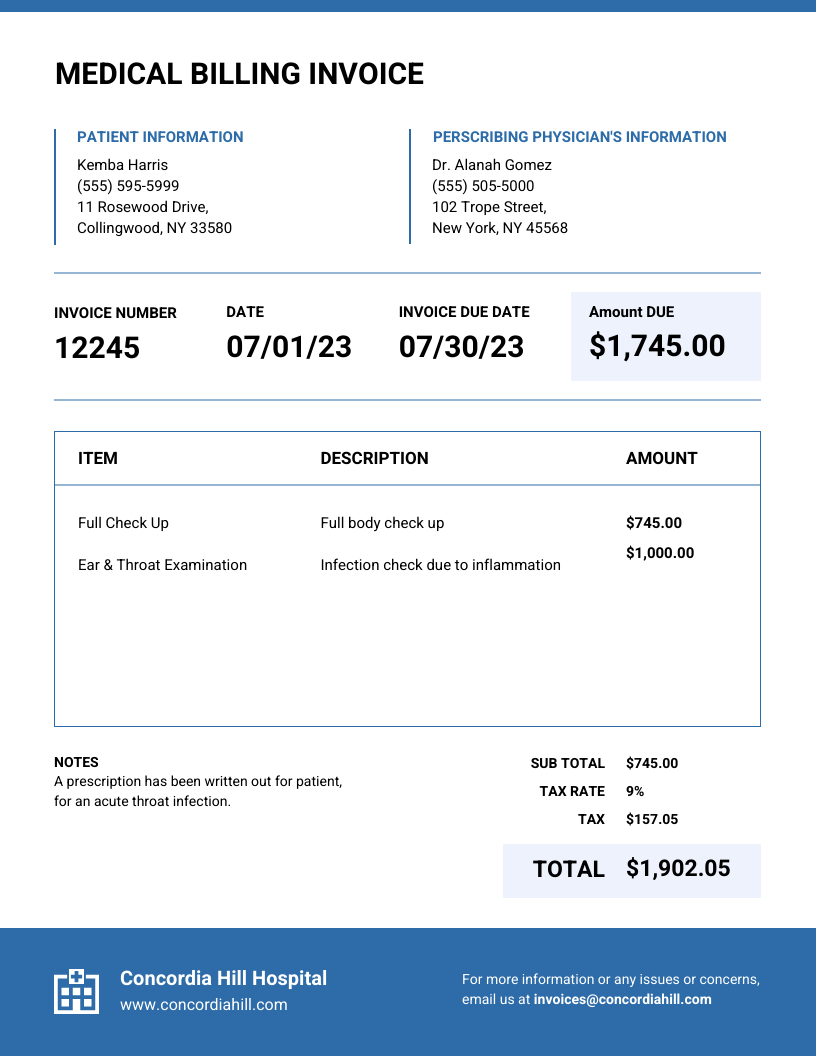
Key Components of a Medical Billing Statement Template
A well-designed medical billing statement template incorporates essential elements to ensure clarity, accuracy, and efficiency in the billing process. These components facilitate transparent communication between healthcare providers and patients, promoting timely payments and minimizing billing disputes. The following components are crucial for an effective template.
1. Patient Information: Accurate patient demographics, including full name, address, date of birth, and contact information, ensure proper identification and facilitate communication regarding billing inquiries.
2. Insurance Information: Details regarding the patient’s insurance provider, policy number, group number, and insured’s name are essential for accurate claims submission and processing.
3. Medical Record Number (MRN): The MRN uniquely identifies the patient within the healthcare system, linking the statement to the patient’s medical record for accurate tracking and reconciliation of services.
4. Date of Service: Accurate dates of service are crucial for tracking patient care, determining appropriate billing, and ensuring alignment with medical records.
5. Service Codes and Descriptions: Utilizing standardized medical codes (e.g., CPT, HCPCS) and clear descriptions ensures accurate billing and facilitates communication between providers, payers, and patients.
6. Charge Amounts: Accurate charge amounts reflect the agreed-upon fees for services rendered, ensuring appropriate reimbursement and maintaining financial integrity.
7. Payment Details: Clear payment instructions, including the total amount due, accepted payment methods, due date, and specific instructions for each method, empower patients to make timely payments.
8. Adjustments and Payments: Documentation of any adjustments made to the charges, such as insurance payments, contractual adjustments, or write-offs, provides transparency and facilitates accurate reconciliation.
These interconnected components form the foundation of a comprehensive and effective medical billing statement. Their presence ensures transparency, accuracy, and efficiency in the billing process, contributing to positive patient-provider relationships and optimized revenue cycle management.
How to Create a Medical Billing Statement Template
Creating a standardized medical billing statement template requires careful consideration of key components and adherence to industry best practices. A well-designed template ensures clarity, accuracy, and efficiency in the billing process, contributing to positive patient-provider relationships and optimized revenue cycle management. The following steps outline the process.
1. Define Essential Information Fields: Begin by identifying the essential data points required for accurate billing and patient identification. This includes patient demographics (name, address, contact information), insurance details (provider, policy number), medical record number (MRN), date of service, service codes and descriptions, charge amounts, and payment details.
2. Select a Template Format: Choose a template format (e.g., spreadsheet, word processing document, specialized billing software) that aligns with existing workflows and technological capabilities. Consider factors such as ease of customization, data integration capabilities, and accessibility features.
3. Design the Layout: Design a clear and organized layout that facilitates easy navigation and comprehension. Group related information logically and use clear headings and labels. Ensure the template adheres to accessibility guidelines for individuals with visual impairments or other disabilities.
4. Incorporate Standardized Codes: Utilize standardized medical codes (e.g., CPT, HCPCS) and descriptions for services rendered. This ensures consistent communication between providers, payers, and patients and facilitates accurate claims processing.
5. Include Clear Payment Instructions: Provide comprehensive payment details, including the total amount due, accepted payment methods, payment due date, and specific instructions for each method. This empowers patients to make timely and accurate payments.
6. Implement Data Validation: Incorporate data validation mechanisms to minimize errors and ensure data integrity. This may involve automated checks for correct formatting, valid code entries, and accurate calculations.
7. Test and Refine: Thoroughly test the template with sample data to identify any potential errors or areas for improvement. Gather feedback from staff and patients to refine the design and ensure usability.
8. Maintain and Update: Regularly review and update the template to reflect changes in industry regulations, coding guidelines, or organizational policies. This ongoing maintenance ensures the template remains compliant and effective.
A well-designed template, incorporating these elements and regularly updated, contributes significantly to accurate billing, efficient revenue cycle management, and positive patient-provider interactions. It provides a framework for clear communication and facilitates timely payment processing.
Standardized medical billing statement templates serve as a crucial communication tool within the healthcare revenue cycle. Accuracy, clarity, and comprehensive information within these documents are essential for efficient processing, timely reimbursements, and positive patient-provider interactions. From patient demographics and service codes to payment instructions and adjustments, each component contributes to a transparent and effective billing process. Implementing robust templates, incorporating data validation mechanisms, and adhering to industry best practices ensures compliance, minimizes errors, and fosters trust between healthcare providers and patients. Effective management of financial processes through well-designed templates strengthens the overall financial health of healthcare organizations.
The evolving landscape of healthcare regulations and technology necessitates continuous adaptation and refinement of billing practices. Commitment to data integrity, standardized processes, and patient-centered communication remains paramount. Embracing technological advancements and prioritizing ongoing evaluation of billing procedures will further optimize revenue cycle management and contribute to a more sustainable and patient-focused healthcare system. Ultimately, the efficacy of medical billing statement templates directly impacts the financial well-being of both providers and patients, underscoring the importance of their meticulous design and implementation.